
The Cancer-Tobacco Link: Using Data to Drive Stronger Tobacco Control Policies
As we observe World Cancer Day today, it is crucial to recognize the significant role smoking plays in the global cancer pandemic. Tobacco use is the leading preventable cause of cancer and cancer-related deaths worldwide, necessitating a dynamic, multidisciplinary approach to tobacco control interventions. DG’s Tobacco Control Data Initiative (TCDI) contains country-specific websites designed to break down barriers to data use in tobacco control by consolidating reliable, comprehensive information on tobacco use, including its impact on cancer.
These 6 country-specific websites provide critical data that reinforces the well-established causal link between tobacco use and cancer, offering a clear, evidence-based picture of the public health threat. The websites feature a wide array of data sources, including primary data collected through TCDI, publicly available secondary data, and peer-reviewed research. By consolidating these resources, TCDI aims to fill existing data gaps and empower stakeholders with the information needed to strengthen tobacco control efforts.
Smoking is the predominant cause of lung cancer cases, responsible for around 85% of all cases worldwide. This is notable given that lung cancer is the principal cause of cancer-related deaths and ranks as the sixth leading cause of death worldwide. Tobacco smoke contains over 7,000 toxic substances, including seven carcinogens that cause cells to grow abnormally, eventually leading to cancer. Even smokeless tobacco, which is chewed, sucked, or sniffed rather than smoked, contains more than 4,000 chemicals—28 of which are known carcinogens. These alarming facts underscore the urgent need for continued awareness and action to reduce tobacco use in the fight against cancer.
Contrary to common beliefs, smokeless tobacco poses significant health risks, often underestimated in comparison to smoking. A single dose of snuff, held in the mouth for about 30 minutes, delivers as much nicotine as four cigarettes, leading to nicotine levels in the blood that can be as high—or even higher—than those from smoking. This makes smokeless tobacco highly addictive, with snuff being even more so than chewing tobacco. Users of smokeless tobacco are at increased risk of developing malignant tumors, particularly in the pancreas, esophagus, and mouth. These risks highlight the severe health consequences of smokeless tobacco, challenging the misconception that it is a safer alternative to smoking.
The Dangers of Secondhand Smoke
There is also a misconception that secondhand smoke is not as harmful as direct smoking. In reality, even brief exposure to passive smoke poses serious health risks to non-smokers. Therefore, there is no safe level of exposure to secondhand smoke, meaning that non-smokers who breathe in secondhand smoke can suffer from serious conditions like coronary heart disease, stroke, and lung cancer. Those living with smokers face a 20% to 30% increased risk of lung cancer due to secondhand smoke’s immediate adverse effects on the cardiovascular system. The dangers extend beyond lung cancer, with evidence linking secondhand smoke to an increased risk of breast cancer, nasal sinus cancer, stroke, atherosclerosis, and even adult-onset asthma.
Similar to active smoking, the longer the duration and the higher the level of exposure to secondhand smoke, the greater the risk of developing lung cancer. These risks underscore the urgent need to protect non-smokers from secondhand smoke in all environments.
Cancer Deaths Attributed to TRIs in TCDI Focus Countries
Tobacco-related illnesses (TRIs) are a significant cause of cancer deaths worldwide, responsible for about 2.6 million cancer deaths in 2019 (the most recent year with available data), highlighting the urgent need for enhanced public health interventions. In Ethiopia, approximately 9,900 deaths are attributed to tobacco use annually, which contributes to a range of cancers as well as cardiovascular and respiratory diseases. Cancer, in general, accounts for 5.8% (2019) of the country’s total mortality, with 1,360 of those deaths directly linked to tobacco use. The cancers most commonly associated with tobacco include lung, laryngeal, esophageal, and oral cancers, among others, emphasizing the wide-reaching impact of tobacco on public health.
Similarly, in Kenya, tobacco-related cancers are responsible for a significant portion of the national cancer burden. A 2022 study, Tobacco Smoking-Attributable Mortality in Kenya, 2012–2021, provides the first comprehensive data on the morbidity and mortality linked to tobacco use in the country. This study found that nearly half (46%) of 2,000 Kenyan patients undergoing cancer treatment had a history of tobacco use, with oral-pharyngeal cancer emerging as the most common tobacco-related illness.
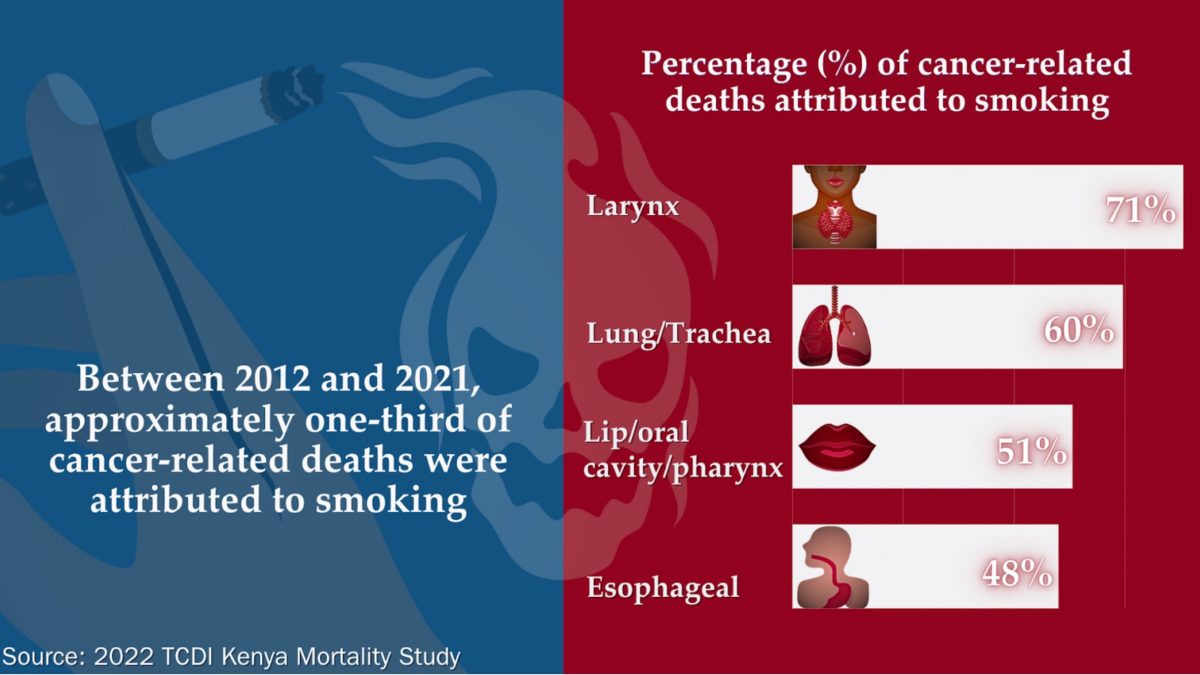
Men were disproportionately affected, making up 91.3% of the 9,934 deaths attributable to tobacco smoking, largely due to higher smoking rates among men.
These findings from both Ethiopia and Kenya underscore the devastating public health toll of tobacco use, particularly in the form of cancer-related deaths, and emphasize the critical need for multidisciplinary, evidence-based tobacco control strategies to reduce its impact.
Treatment and Healthcare Costs
TRIs not only devastate public health but also impose a heavy economic burden. According to Kenya’s 2022 study, the cost of treating patients with these illnesses is staggering, with lung cancer leading the way at $23,365 per case, followed by oral-pharyngeal cancer at $7,637. The majority of these costs stem from expenditures on medicine and medical staff. While cancers incur the highest treatment costs per case, they contribute less to overall healthcare spending compared to cardiovascular diseases. This is primarily because most cancer cases are diagnosed at advanced stages, limiting treatment options and resulting in poor outcomes and high fatality rates.
The Centre for the Study of the Economies of Africa’s (CSEA) study, Health Burden and Economic Costs of Tobacco Smoking in Nigeria, found that in 2019, 29,474 deaths were attributable to smoking, and the Nigerian healthcare system spends 526.4 billion Naira (the equivalent of USD 1.71 billion in 2019 NGN) in treating TRIs, annually. Researchers found that if the price of cigarettes were to increase by 50%, 23,838 deaths would be forestalled and the government would benefit from healthcare cost savings and increased tax revenue collection.
In 2021, TRIs in Kenya were responsible for significant economic losses, yet the revenue generated from the tobacco industry—through taxes and other contributions—covered only 63.8% of the estimated healthcare expenditures caused by tobacco use. This stark gap between the costs of treating TRIs and the revenues from tobacco taxation underscores the unsustainable economic impact of tobacco consumption.
Policy Recommendations for Public Health Interventions
Reducing cancer deaths linked to tobacco-related illnesses requires a dynamic, multidisciplinary approach to tobacco control that adapts to the political, socioeconomic, and cultural context of each region. Several strategies are essential across all six TCDI focus countries—Zambia, South Africa, Kenya, Ethiopia, DRC, and Nigeria. First, reinforcing the implementation of the Framework Convention on Tobacco Control (FCTC) to reduce tobacco use prevalence.
Alongside this, robust cessation programs must be integrated into diverse settings, including health facilities, workplaces, higher education institutions, and communities, to reach individuals across various stages of life and socio-economic backgrounds. Given that tobacco use is responsible for far more cancers than other adjustable behaviors– like consuming alcohol or physical inactivity–interventions aiming to help individuals quit smoking could have the most significant global impact on cancer prevention.
Gender mainstreaming is also vital; tobacco control policies and interventions should be designed with a gender perspective, recognizing the differing prevalence of tobacco use and associated health outcomes between men and women.
Further, comprehensive data collection is necessary to assess and monitor the tobacco epidemic effectively. This includes systematically gathering data on both morbidity and mortality rates related to tobacco use, such as the incidence of lung cancer, cardiovascular diseases, and respiratory disorders. In addition to clinical data, there should be linkages between electronic health records and national registries to enable real-time monitoring and trend analysis. Surveys and population-based studies can also provide insights into tobacco use patterns, including initiation, cessation rates, and the social determinants influencing tobacco consumption. This robust data collection will allow for consistent, evidence-based policy adjustments and interventions, ensuring that strategies to reduce tobacco use are responsive to local context and effective.
Expanding the scope of research to include tobacco-related morbidity, mortality, and the economic impact of diseases not covered in existing studies will offer a more complete picture of the toll of tobacco. Equally important is the responsible management of tobacco funds—resources collected from the tobacco industry should be used prudently to finance cessation programs and support healthcare costs associated with treating tobacco-related illnesses.
Finally, progressively increasing tobacco taxes remains one of the most effective tools to reduce consumption and alleviate the financial burden on healthcare systems. By combining these efforts into a cohesive, integrated approach, countries can make significant strides in reducing the devastating impact of tobacco use on public health.