Streamlining Doctor-Patient Communication to Personalize Care
Abdoulaye Bagaya, a DCDJ Fellow in Côte d’Ivoire, developed an app for FSU COM Abobo Sagbe Hospital during his 7-month internship placement. The app helps community counselors, healthcare assistants, and clinic counselors manage patient contact and treatment information.
Background
The Des Chiffres et Des Jeunes (DCDJ) Data Fellowship is a flagship DCDJ program that places technically-trained Ivorian youth into organizations where they encourage and increase the degree to which data is used for decision making. DCDJ is a program led by Development Gateway and funded by the Data Collaboratives for Local Impact (DCLI) program. The DCDJ Data Fellowship builds young peoples’ skills to strategically catalyze sustainable change, and DCDJ as a whole leverages local capacity to improve data access, sharing, and availability.
Abdoulaye Bayaga, a DCDJ Fellow, used his 7-month internship at a hospital in Abobo, Côte d’Ivoire to build a tool that helps doctors and healthcare facilities more easily contact patients and track their medical history. This helps the hospital save time, stay in closer touch with patients, and ultimately reduce Interruption in Treatment (IIT) cases.
Problem
Before Abdoulaye arrived at the hospital in Abobo, healthcare workers would manually look up phone numbers to call about 60 patients per day before their appointments. This process involved searching through hard copies of patient files, paperwork, and other information to find patients’ records and contact information – sometimes unsuccessfully. The hospital’s community counselors were the ones burdened with managing nearly 800 total patients, tracking down contact information, and calling patients.Without contact from the hospital, patients are left largely to themselves, expected to be engaged in their care sufficiently to own and manage their medical conditions in a timely manner.
Underscoring this challenge, community counselors were not the only ones working with the patient records – doctors and other administrative staff would all regularly handle the same physical records. It was difficult for multiple people to reference the same information at the same time when only one physical copy of the record was available.
Solution
Abdoulaye assessed this situation at the site, identifying the main challenge was that community counselors were having a hard time finding patient contact information to confirm appointments. This was often because another person would be holding the physical file, or because the file was simply misplaced or lost.
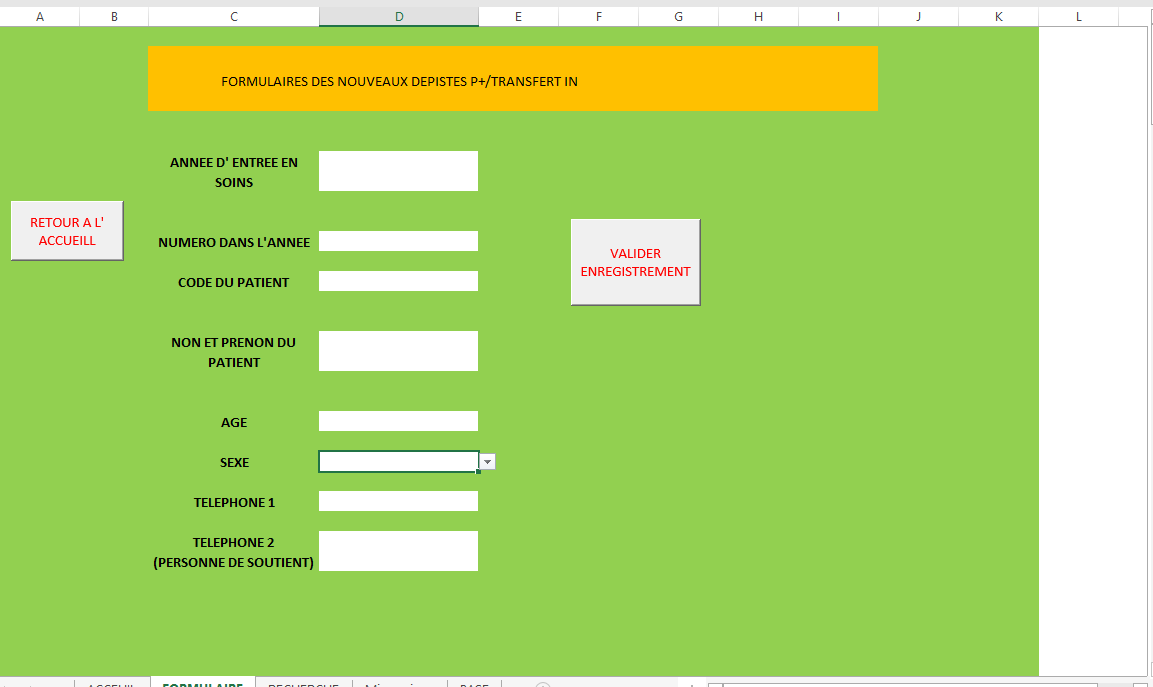
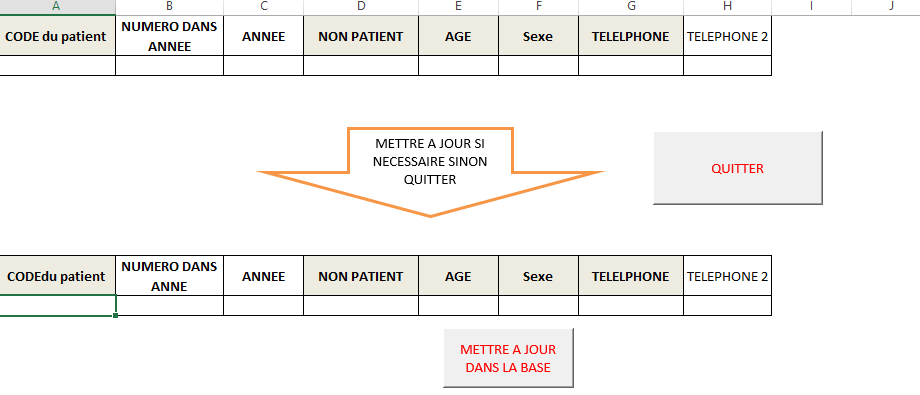
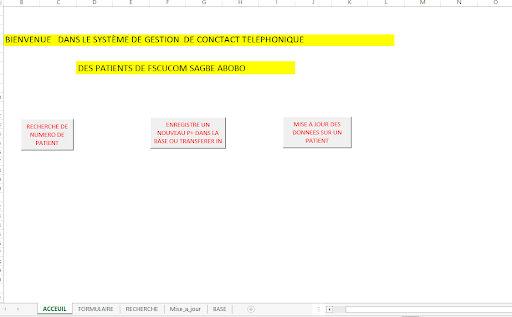
Abdoulaye came up with a tool that would digitize the name and phone number of the patients – enabling counselors to more easily contact patients whenever they would miss appointments.
Processes
Abdoulaye used Excel and Microsoft Visual Basic to develop the tool. He focused on two easy-to-use methods that community counselors – less familiar with complex technical solutions – would be able to integrate into their daily work. He also completed in-depth training and a webinar tutorial for community counselors to use the tool independently. Because of Covid-19, additional in-person training could not be completed; however, the webinar tutorial was an easy, remote alternative that empowered counselors to be trained on their own time, on their own schedules.
Outcomes and Impacts
First and foremost, the tool optimizes community counselors’ time at the hospital. Before the tool, it would take 1-2 days for counselors to gather all the contact information to call patients. Now, thanks to the app, needed information is ready in 25-30 minutes. Instead of spending days collecting information, they have been dedicating their saved time to home visits with patients, delivering medications, and providing personalized care. With increased home visits, community counselors can better ensure patients are taking their medications daily. Additionally, they can focus on health promotion, reducing HIV/AIDS stigma, and providing advice to people who have been recently diagnosed with the disease. These patient home visits, supporting mental wellbeing, and as Abdoulaye put it, “letting [newly diagnosed patients] know it isn’t the end of the world, and that their lives will continue on.”
Conclusion
Instead of having to continuously search for patient records to track down their contact information, community counselors can now pay special attention to personalized healthcare – essential for HIV/AIDS positive patients – to ensure they continue to seek the care they need. According to NIH research publications, home visits decrease costs, improve health outcomes, and reduce hospital stays. Not only has Abdoulaye’s tool drastically changed the way this Abobo hospital is able to provide care, Abdoulaye himself learned a lot during the process. As a statistician by trade, he can now use a wider range of technical tools and machine learning algorithms to analyze data, build dashboards, and support decision-making. Moving forward, in addition to continuing his endeavors in healthcare data use, he also plans to take his knowledge gained as a DCDJ Fellow to the fiscal and tax industry as well.