Tobacco Cessation: Another Tool for Governments Fighting Coronavirus?
As the global community scrambles to better understand why Covid-19 can impact individual patients so differently, a growing body of evidence suggests that one factor contributing to the severity of the disease is whether the patient is a smoker. Other early reports indicate that vaping could have a similar effect (for example, the University of California San Francisco recently added smoking or vaping as a risk factor to its recommended screening protocol for Covid-19 patients).
Despite warnings from public health officials, smokers do not seem to be adjusting their behavior in response: in fact, demand for cigarettes has increased. Even more concerning, downloads of smoking cessation apps actually decreased in March.
We are now seeing healthcare systems around the world groan under the influx of patients suffering from severe cases of coronavirus. The virus’s impact is likely to be even worse on health infrastructure in the global south, where the challenge of responding in a low-resource setting will be exacerbated by having very little data about the prevalence of infections in-country.
Development Gateway (DG)’s Tobacco Control Data Initiative (TCDI), funded by the Bill & Melinda Gates Foundation, is based on the knowledge that when the right information is available, governments are able to make effective, evidence-based policy decisions to limit tobacco use and monitor those implemented policies. While a limited amount of concrete data on the virus exists, and public health efforts are laser-focused on reducing the burden on healthcare systems, reducing smoking could be a strong option for Covid-19 risk reduction.
It makes sense that country governments might seek to limit tobacco use during this ongoing health crisis, expecting that fewer smokers could mean fewer cases of coronavirus that become severe enough for hospitalization. In fact, this is exactly what some governments are beginning to do: South Africa has banned sales of cigarettes, and the city of Thane, outside Mumbai, has banned sales of all tobacco products, to reduce both smoking and spitting. In the US, similar propositions are under consideration: the US House Oversight Committee has requested that the FDA ban e-cigarettes because of the coronavirus link, and the New York State Academy of Family Physicians is urging the governor issue an executive order banning the sale of tobacco products.
The potential impact of anti-smoking interventions in the medium term is strong beyond the immediate need to “flatten the curve.” As experts suspect, rates of Covid-19 infection are likely to decrease in the summer and increase again in the fall and winter. If this holds true, it means that there is an upcoming window of time for countries to ramp up their smoking cessation efforts to limit that resurgence come the colder seasons. As an example of potential action, in the UK, people can access clinics for quitting smoking through the National Health Service (NHS), the publicly-funded UK health system. In the next few months, the UK could increase funding for those clinics and invest in advertising that emphasizes the link between smoking and the risk of developing a severe case of Covid-19.
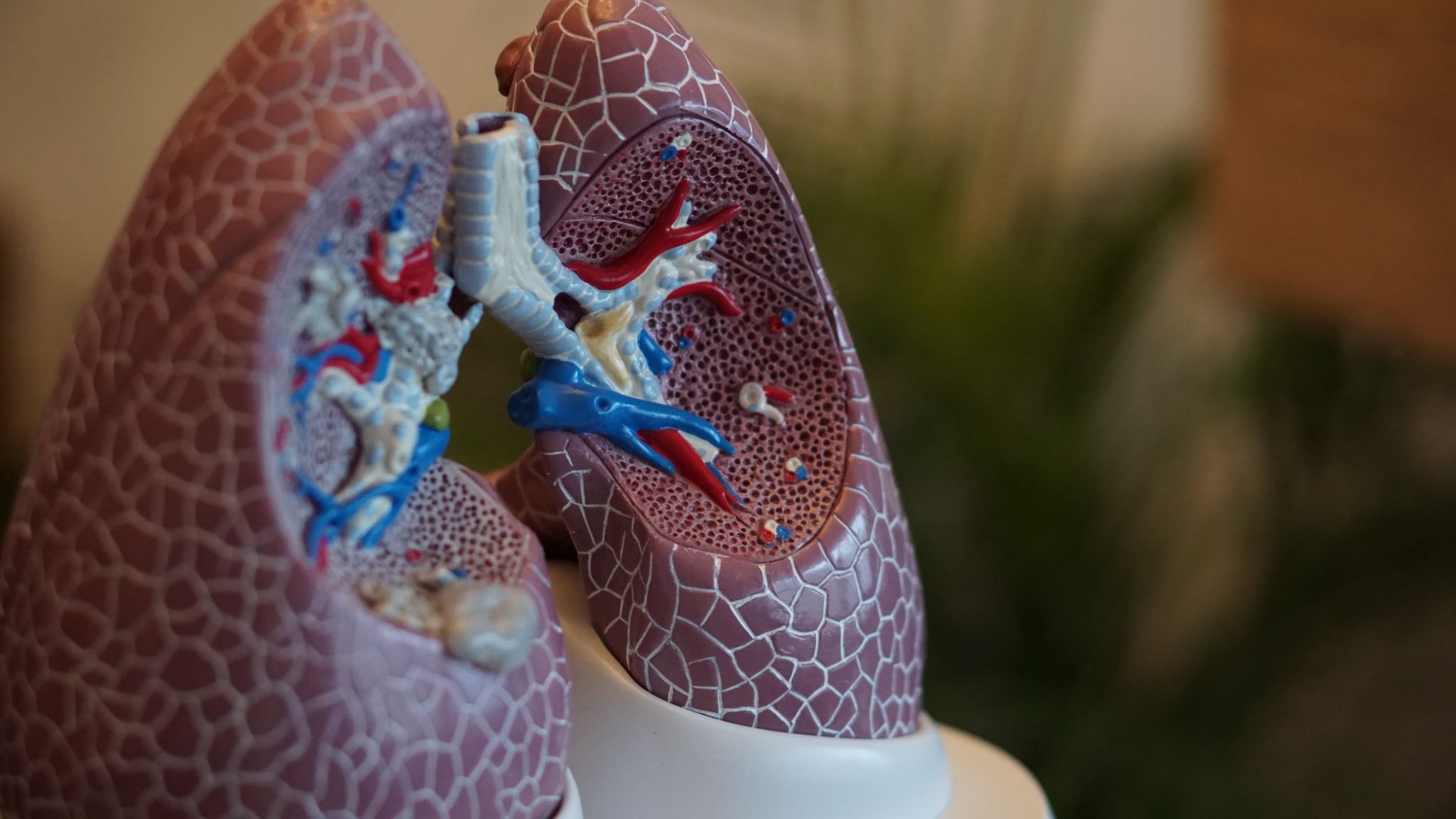
Through our work on TCDI, DG understands the challenges involved in strengthening tobacco control programs in countries with limited funding for that type of programming. However, this moment may prove to be quite timely for governments to invest in a concerted effort to pair stricter tobacco control policies with focused public health messaging. Smokers may be far more likely to change their behavior if they know, for instance, that a small study in China indicated smokers who had coronavirus were 14 times more likely to have their infection progress or even become fatal; or that the damage to lungs begins repairing immediately upon quitting. Additionally, for different users, there could be high value in information like the fact that nicotine replacement therapy (such as nicotine patches and lozenges) does not carry the coronavirus-related risks of smoking or vaping.
Given the complex factors at play, there is potential for tobacco control to have a significant impact on Covid-19 hospitalization rates and even mortality. If rates of other smoking-related deaths drop as well, that’s even better yet.
Photo credit: Robina Weermeijer on Unsplash
Share This Post
Related from our library
Data on Youth and Tobacco in Africa Program Enters Phase II
The Data on Youth and Tobacco in Africa (DaYTA) program is launching its second phase, expanding to five additional countries. This blog highlights DaYTA’s objectives, innovative approach, and the key activities driving impact in adolescent tobacco control measures.

From Standardization to Specificity: Localizing Multi-Country Research
Multi-country research must balance consistency with local realities. While standardization allows reliable comparisons and generalizable insights, local context shapes outcomes. This blog explores how programs can strike that balance effectively.

Harnessing the Power of Data: Tackling Tobacco Industry Influence in Africa
Reliable, accessible data is essential for effective tobacco control, enabling policymakers to implement stronger, evidence-based responses to evolving industry tactics and public health challenges. This blog explores how Tobacco Industry strategies hinder effective Tobacco control in Africa, and highlights how stakeholders are harnessing TCDI Data to counter industry interference.